Headaches
Classification of orofacial pain
(see Classification Tables)
The aim of this section is to outline the causes of chronic orofacial pain (lasting >3 months). However, the most common causes of acute dental pain are trauma or infection of the dental pulp which contains the nerves and vessels supplying the tooth. There is a substantial cross over between orofacial pain and headaches largely due to both causing pain within the trigeminal system – see more here.
Chronic orofacial pain
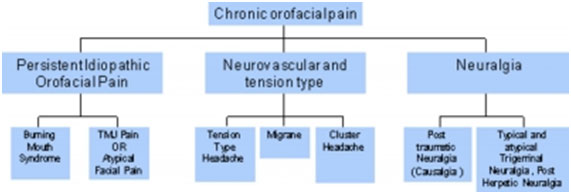
Several classifications of chronic orofacial pain have been presented and they do conflict with each other. The author will use the mechanistic based classification by Woda et al for this chapter as it presents a pragmatic and clinically useful tool
Fig. 1 Chart illustrating a suggested classification for chronic orofacial pain.
 Group 1: Neurovascular (predominantly ophthalmic division [V1] pain)
Group 1: Neurovascular (predominantly ophthalmic division [V1] pain)
Headache is a common condition, which accounts for around 4% of all consultations in primary care—around 6 million people in the UK are affected by migraine, and, at any one time, 40% of the population have tension-type headache. In November 2008, SIGN published a full guideline and quick reference guide on the Diagnosis and management of headache in adults. Prior to this, the main pieces of guidance available to the UK physician for the management of headache included:
- comprehensive diagnostic criteria from the International Headache Society (IHS)
- evidence-based criteria from the Migraine in Primary Care Advisors (MIPCA) guidelines on the management of migraine, and chronic headaches
- consensus-based criteria from the British Association for the Study of Headache (BASH) on the management of migraine, tension-type headache (TTH), cluster headache, and medication overuse headache (MOH).
- Although collectively these documents provided comprehensive guidance, it was not always consistent or user-friendly for the physician managing a patient with headache. The SIGN guideline, which has incorporated material from the three sources listed above, may therefore have the potential to become the ‘one-stop’ source of information on headache for the physician. In this article I have provided my personal view on how well the SIGN guideline fulfils this requirement.
- Links to associations with information and patient support
-
- Patient choice NHS http://www.nhs.uk/Conditions/Headache/Pages/Introduction.aspx
- Patient UK http://www.patient.co.uk/doctor/headache-pro
- Migraine trust http://www.migrainetrust.org/
- Migraine Action http://www.migraine.org.uk/
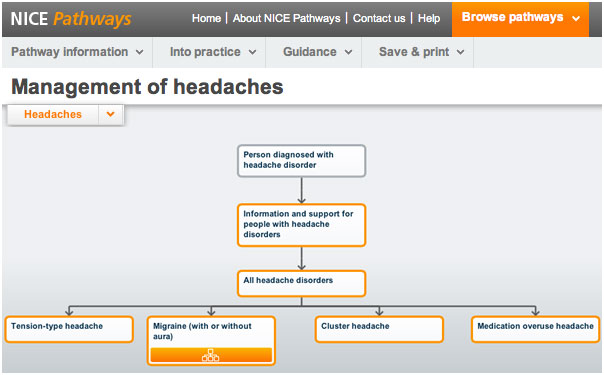
Clinical pathways have been established with patient pathways.
Migraine
Migraines are perhaps the most studied of the headache syndromes. This is due in part to the high incidence and significant loss of productivity and limitation on quality of life suffered by those with the syndrome. It is estimated that 17% of women and 6% of men have migraine headaches. Onset is usually in the second or third decade.
Characteristics of migraine include:
- Five or more lifetime headache attacks lasting 4–72 hours each and symptom-free between attacks, moderate to severe pain, unilateral with or without aura visual signs.
- The female-to-male ratio is 3:1.
- It is unilateral but can be bilateral.
- The pain has a throbbing quality and feels as if it is associated with a pulse.
- Photophobia, phonophobia, and osmophobia are features of migraine, as is nausea.
- The pain worsens with exertion and improves with sleep.
- The patient may or may not experience aura.
Pharmacological therapy includes abortive and preventative medications, depending on the frequency and severity of the headaches. Abortive agents include serotonin agonists, ergotamine, isometheptene, and anti-inflammatories. Preventative agents
include antiepileptic drugs (AEDs), beta-blockers, calcium channel blockers, tricyclic antidepressants (TCAs), selective serotonin reuptake inhibitors (SSRIs), and angiotensin receptor blocking agents.
Tension-type headaches
Tension-type headache (TTH) is the most common type of headache. It occurs in 69% of men and 88% of women over a lifetime, and the annual prevalence is 63% in men and 88% in women. TTH can be further be distinguished as ‘episodic’ TTH (ETTH) or ‘chronic’ TTH (CTTH). The distinction is made largely on frequency of occurrence (<15 days a month for Migraine and > 15 days a month for TTH).
Characteristics of tension-type headache include:
- Highest socioeconomic impact, affecting 30–78% of the population.
- At least 10 episodes, occurring less than one day a month on average.
- Infrequent episodes lasting from 30 minutes to seven days.
- Typically bilateral.
Medication overuse headaches
This is a newly-recognised phenomenon that may characterise the majority of headache patients in the West (30–78%). It is recognised that long term ingestion of over-the-counter analgesics can result in a compromised pain resistance.
Chronic daily headache
Chronic daily headache (CDH) is described as headache occurring at least six days a week for a period of at least 6 months. The pain is usually present throughout the day with little time spent pain-free. The head pain is typically bilateral, frontal or occipital, non-throbbing and moderately severe. The syndrome is associated with the overuse and abuse of many common over-the counter pain medications (aspirin, acetaminophen, ibuprofen, etc.), barbiturates, and opioid analgesics. A careful history will reveal an increasing need for medications and the emergence of a chronic headache that is qualitatively distinct from the headache for which it was originally taken. This led to the idea of CDH being a ‘transformed migraine’.
Trigeminal autonomic cephalgias
https://ouchuk.org/ is the charity providing excellent patient support and advice for these conditions (including Cluster headache and short lasting unilateral neuralgiform headache attacks with conjunctival injection and tearing (SUNCT))
Cluster headache (CH) is characterised by intensely severe pain (sometimes termed suicide headache) with boring or burning qualities located unilaterally in the orbital, supraorbital, or temporal area.
Characteristics of cluster headaches include;
- The male:female ratio is 6:1.
- The onset of pain is sudden.
- Unilateral orbital, supraorbital or temporal.
- Severe episodic pain lasting 15-180 minutes.
- Up to eight times a day to every other day for a period of 2-12 weeks.
- The pain is characterized as severe, boring, and burning.
- It awakens the patient from sleep and does not improve with rest. Many individuals pace and may injure themselves because of the severity of the pain.
- Associated symptoms include ipsilateral conjunctival injection, tearing, and nasal congestion.
Management Abortive treatment includes oxygen, sumatriptan injections, and/or dihydroergotamine. Preventative treatment includes verapamil, lithium, divalproex sodium, and topiramate.
Short-lasting unilateral neuralgiaform conjunctival irritation and tearing (SUNCT) is possibly a variation of the cluster tic syndrome. It is characterized by brief (15–120 seconds) bursts of pain in the eyes, temple, or face. The pain is usually unilateral and is described as burning, stabbing, or electric. It occurs frequently in a 24-hour period (>100 episodes). Neck movements can trigger the pain. SUNCT syndrome is refractory to medical therapy but there is increasing evidence for treatment with lamotrigine.11
Giant cell arteritis Temporal arteritis
Please see information and leaflet.
Temporal arteritis is characterised by daily headaches of moderate to severe intensity, scalp sensitivity, fatigue, and various non-specific complaints with a general sense of illness. Ninety-five per cent of patients are over 60 years old.12 The pain is usually unilateral, although some cases of bilateral or occipital pain do occur. Pain may also be felt in the tongue and is a continuous ache with superimposed sharp, shooting head pains. The pain is similar to and may be confused with that of CH, but CH tends to occur in younger patients. The two may also be distinguished on physical exam, when dilated and tortuous scalp arteries are noted. The erythrocyte sedimentation rate (ESR) is markedly elevated in temporal arteritis. Definitive diagnosis is made by artery biopsy from the region of the pain, although negative biopsy may be caused by the spotty nature of the disease and does rule out the diagnosis. High dose steroid therapy usually precipitates a dramatic decrease in head pain. Failure to respond to steroid therapy with a negative biopsy should call the diagnosis into question. If the diagnosis seems likely based on history and physical examination, steroids should be started immediately to avoid vision loss, the most common complication of the disorder, occurring in 30% of untreated cases. The biopsy remains positive for 7–10 days from starting steroid therapy. Steroids may be tapered to an every other day maintenance schedule when the pain resolves and ESR normalizes. The disease is usually active for 1–2 years, during which time steroids should be continued to prevent vision loss.
Useful links
- Trigeminal autonomic cephalgias
- Ouch https://ouchuk.org/
- Headaches
- Patient choice NHS http://www.nhs.uk/Conditions/Headache/Pages/Introduction.aspx
- Patient UK http://www.patient.co.uk/doctor/headache-pro
- Migraine trust http://www.migrainetrust.org/
- Migraine Action http://www.migraine.org.uk/
- orofacial pain
- https://learningcentral.cf.ac.uk/bbcswebdav/courses/MEDIC-PCA-BBTRAIN/Dental/diagnosis_treatment_non_dental_facial_pain/diagnosis_treatment_non_dental_facial_pain_print.html
- https://learningcentral.cf.ac.uk/bbcswebdav/courses/MEDIC-PCA-BBTRAIN/Dental/diagnosis_treatment_non_dental_facial_pain/diagnosis_treatment_non_dental_facial_pain_print.html
- Treatment
- Self help guide for chronic pain sufferers http://www.moodjuice.scot.nhs.uk/chronicpain.asp
- Tricyclic antidepressants http://www.patient.co.uk/health/tricyclic-antidepressants
- Pregabalin http://www.patient.co.uk/medicine/Pregabalin.htm
- Gabapentin http://www.patient.co.uk/medicine/gabapentin-neurontin
- Venlafaxine http://www.patient.co.uk/medicine/venlafaxine
- Duloxetine http://www.patient.co.uk/medicine/duloxetine-for-mood-and-nerve-disorders
- Oxcarbazepine http://www.patient.co.uk/medicine/Oxcarbazepine.htm
- Lamotrigine http://www.patient.co.uk/medicine/Lamotrigine.htm
- Baclofen http://www.patient.co.uk/medicine/baclofen-for-chronic-muscle-spasm-lyflex-lioresal
- Opioid pain killers http://www.patient.co.uk/health/strong-painkillers-opioids
- Support for chronic pain patients
- Action on Pain www.action-on-pain.co.uk PO Box 134, Shipdham, Norfolk, IP25 7XA Tel: (Painline) 0845 603 1593. Action on Pain is a national charity, run by volunteers, the majority of whom have chronic pain, which provides support and information for people affected by chronic pain, either as a sufferer or a carer/relative. They are a strong lobbying organisation working hard to increase the provision of effective pain management services within the NHS and are an independent, non-political organisation focussed clearly on the key issues around pain management. They promote the positive side of effective pain management whenever possible in order to improve the quality of life for people in chronic pain. As well as the Painline they have a mobile information unit and an effective range of informative publications.
- Chronic pain coalition www.paincoalition.org.uk. c/o Policy Connect
CAN Mezzanine, 32-36 Loman Street, Southwark, SE1 0EH Tel: 0207 202 8585. The Chronic Pain Policy Coalition is a forum established in 2006 to unite patients, professionals and parliamentarians in a mission to develop an improved strategy for the prevention, treatment and management of chronic pain and its associated conditions - The neuropathy trust www.neurocentre.com PO Box 26, Nantwich, Cheshire, CW5 5FP. The Neuropathy Trust is a worldwide Charity and was founded in 1998 to provide a lifeline to people affected by Peripheral Neuropathy (PN) and Neuropathic Pain (NeP). It is the primary function of the Trust to ensure, irrespective of the cause of the peripheral neuropathy or neuropathic pain (whether known or otherwise) that patients, family, carers and health care providers receive the highest possible level of information and support. The Neuropathy Trust is independent of any government, political ideology, economic interest or religion.
- Pain concernwww.painconcern.org.uk Unit 1-3, 62-66, Newcraighall Road, Fort Kinnaird, Edinburgh, EH15 3HS Tel: (Helpline) 0300 123 0789 (10 am-4 pm, Monday-Friday), (Admin) 0131 669 5951
- Information and support for pain sufferers, those who care for them and about them.
- Free factsheet and leaflets to help you manage your pain.
- Quarterly magazine.
- Listening-ear helpline – the chance to talk to another pain sufferer (see Contact Us).
- Online forum.
- An internet radio programme, Airing Pain, which includes Q and A sessions and interviews with patients and professionals
- Patient diaries
- Online migraine diary http://diary.migrainetrust.org/
- Pain professional support https://healthskills.wordpress.com/2011/07/01/what-is-this-thing-called-pain/
- Professional organisations
- International Headache society (HIS) http://www.ihs-headache.org/
- British pain society(BPS) http://www.britishpainsociety.org/
- European academy of craniomandibular disorders (EACDS) http://www.eacmd.org/
- international association for the Study of Pain (IASP) http://www.iasp-pain.org/
- Grunenthal change pain site for professional and patients http://www.change-pain.co.uk/
- American academy of orofacial pain (AAOP) v http://www.aaop.org/
- British Association of Oral Surgeons (BAOS) http://www.baos.org.uk/Resources.cfm#2
- Royal college of anaesthetists faculty of pain
- British dental association
- International association of oral and maxillofacial surgery
- British dental journal
- Dental update
- NHS patients advice pain management, toothache, headaches, PHN, wisdom teeth http://www.patient.co.uk/symptom-checker
Education menu

Physiotherapy for Orofacial Pain
A short introductory presentation by Dr Hedvig van der Meer who has recently joined our team:

Our guide to better sleep
By Georgina Gray Good quality sleep is one of our core health pillars. Not only is it vital for energy, mental health and hormone production, it is also important for disease prevention and weight control. We should be aiming for 7-9 hours of good quality sleep every...

